Heart Under Siege: The Cardiovascular Risks of Air Pollution
Introduction
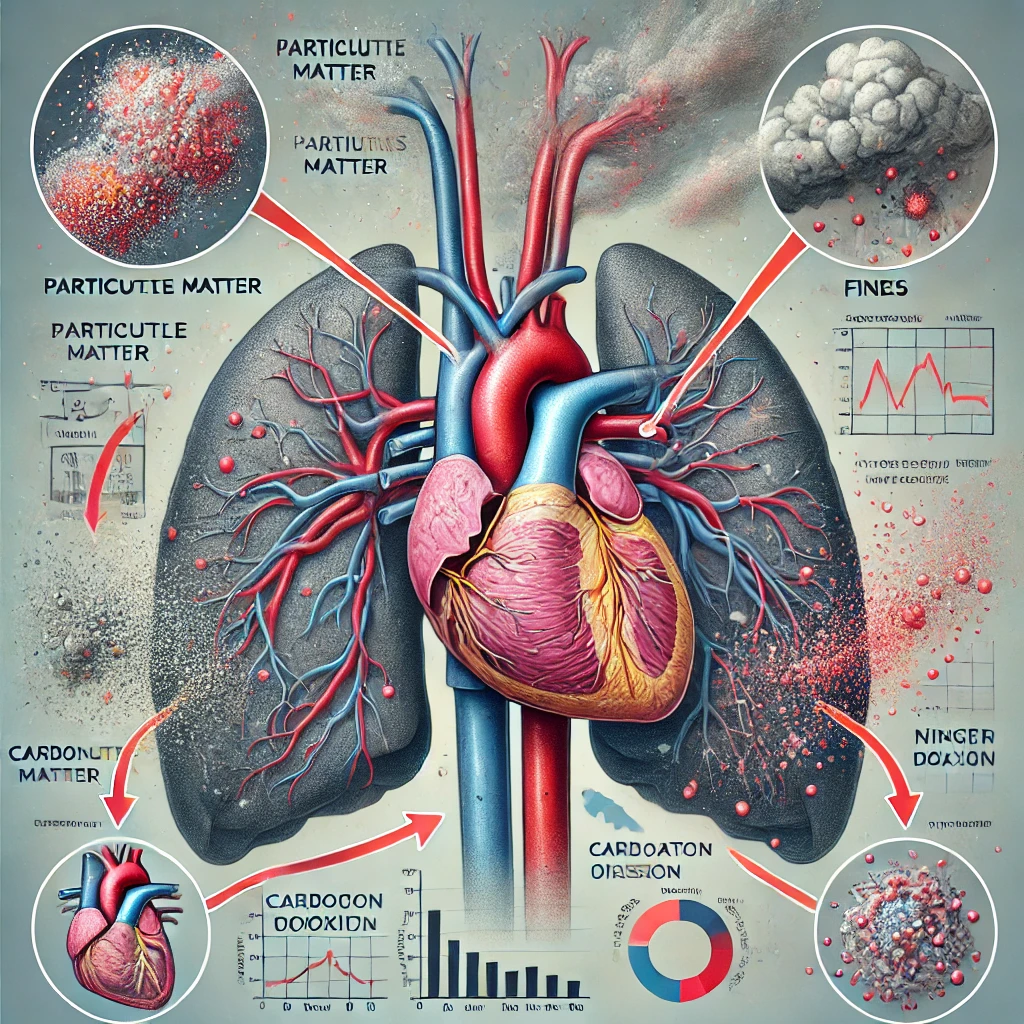
Air pollution poses a significant health risk, impacting not only respiratory health but also cardiovascular health. Initially, the focus was primarily on the harmful effects of smog and air pollution on the respiratory system. However, recent studies reveal that cardiovascular diseases account for the majority of pollution-related mortality.
Research shows that exposure to certain pollutants correlates with increased mortality rates. Specifically, long-term exposure to fine particulate matter (PM2.5) and short-term exposure to coarse particulate matter (PM10) are linked to serious health risks. Air pollution is associated with several cardiovascular conditions, including acute myocardial infarction, heart failure, cardiac arrhythmias, atherosclerosis, and even cardiac arrest.
Addressing this issue requires strong environmental regulations, but individuals can also take steps to reduce their risk. Staying indoors on high pollution days and considering the use of a face mask, particularly when particulate matter levels are high, can help minimize exposure. While the use of masks remains debated, they may offer protective benefits under certain conditions. (1)
Health Risks Linked to PM2.5 Exposure: Findings from the American Cancer Society
According to data from the American Cancer Society (ACS) cohort, a 10 μg/m³ increase in annual average exposure to fine particulate matter (PM2.5) is associated with a notable rise in mortality rates. Specifically, long-term all-cause mortality increases by approximately 4%, cardiopulmonary mortality by 6%, and lung cancer mortality by 8%. These findings underscore the serious health risks posed by PM2.5 exposure and highlight the importance of minimizing air pollution exposure to protect public health. (2)
Link Between PM2.5 and Acute Myocardial Infarction (AMI) Onset
To assess whether high concentrations of ambient particulate matter can trigger acute myocardial infarction (AMI), Peters and colleagues conducted a case-crossover study as part of the Determinants of Myocardial Infarction Onset Study. They interviewed 772 AMI patients, analyzing exposure to PM2.5. The study found that elevated PM2.5 concentrations were linked to a heightened, short-term risk of AMI onset, particularly within two hours and up to one day following exposure. This research highlights the potential for fine particulate matter to act as a trigger for heart attacks in vulnerable individuals. (3)

Potential Mechanisms Linking Air Pollution to Cardiovascular and Respiratory Diseases
Impact of Combustion Particles on Heart Rate Variability and Cardiac Health
Animal studies indicate that exposure to combustion particles can reduce heart rate variability, a measure of cardiac autonomic function. Reduced heart rate variability is associated with disruptions in the autonomic nervous system, which regulates heart rhythms. This alteration in cardiac function is considered a significant risk factor for sudden cardiac death and fatal arrhythmias, highlighting the potentially deadly impact of air pollution on heart health. (4)(5)(6)
Research in humans has confirmed the cardiac effects of air pollution seen in animal studies. In the German MONICA (MONItoring of trends and determinants in CArdiovascular disease) study, heart rates were found to increase with higher concentrations of sulfur dioxide (SO₂) and carbon monoxide (CO). These findings suggest that exposure to certain air pollutants can elevate heart rates, potentially placing individuals at greater risk for cardiovascular events. (7)
Three studies conducted in the United States, including a total of 54 subjects, found a reduction in heart rate variability with the increases of PM10 or PM2.5. (8)(9)(10)
ACS Cancer Prevention II Study: Linking Fine Particulate Matter to Mortality
The largest study to date on the effects of air pollution, the ACS Cancer Prevention II study, enrolled nearly 500,000 individuals over a 16-year period. Findings showed that each 10 μg/m³ increase in fine particulate matter (PM2.5) was associated with increases in all-cause mortality by 4%, cardiopulmonary mortality by 6%, and lung cancer mortality by 8%.
These findings suggest that impaired cardiac autonomic function may serve as a critical link between air pollution and cardiovascular mortality, potentially triggering fatal tachyarrhythmias and contributing to increased risk of sudden cardiac death in polluted environments.
Air Pollution’s Role in Cardiovascular Health Risks
Acute myocardial Infection
Exposure to particulate matter, specifically PM10 and PM2.5, has been shown to cause systemic oxidative stress and inflammation, along with elevated serum fibrinogen levels. These changes contribute to increased platelet reactivity, endothelial dysfunction, and plaque instability—factors that heighten the risk of cardiovascular events. Studies have also linked PM10 exposure to the triggering of acute myocardial infarction (AMI), underscoring the serious cardiovascular risks posed by air pollution. (11)
Heart failure
The connection between smog exposure and heart failure is less immediately apparent, but the underlying mechanism involves a supply-demand mismatch in the heart. Increased heart rate, elevated blood pressure, and higher filling pressures can all contribute to this mismatch. Additionally, reduced contractility and increased myocardial injury due to air pollution further exacerbate the strain on the cardiovascular system, potentially triggering or worsening heart failure.
Arrhythmias
A study conducted in São Paulo investigated the relationship between environmental pollution and the occurrence of arrhythmias that required emergency department visits. The study found a significant association between increases in carbon monoxide (CO), nitrogen dioxide (NO₂), and particulate matter (PM10) and the occurrence of various arrhythmias. These included sinus tachycardia, atrial fibrillation (AF), atrial flutter, supraventricular tachycardia, and ventricular tachycardia and fibrillation. The findings highlight the impact of air pollution on heart rhythm disturbances, underscoring the cardiovascular risks of exposure to these pollutants. (12)
Predisposition to Risk from Air Pollution
Not everyone is equally affected by air pollution; certain groups are more vulnerable due to preexisting health conditions. There is a significant correlation between air pollution exposure and individuals with cardiovascular problems, diabetes, impaired glucose tolerance, smoking habits, age, and chronic obstructive pulmonary disease (COPD). These populations are at a higher risk of experiencing severe health effects from air pollution, highlighting the need for targeted public health strategies to protect these vulnerable groups. (13)
Cardiac arrest
A study conducted in Rome involving over 5,000 individuals found that exposure to particulate matter (PM) and carbon monoxide (CO) were predictive of sudden cardiac arrest. The research highlighted that elderly individual (aged >65 years), those with hypertension, and individuals with chronic pulmonary diseases were particularly predisposed to experiencing sudden cardiac arrest due to air pollution exposure. These findings underscore the heightened cardiovascular risks faced by vulnerable populations living in polluted environments. (14)
Congenital heart
An American study found a direct relationship between exposure to carbon monoxide (CO) and the occurrence of ventricular septal defects. Additionally, elevated levels of ozone (O₃) were correlated with valvular, truncal, and aortic defects. However, no significant correlation was found between particulate matter (PM) or other pollutants and these specific types of cardiac defects. These findings highlight the potential role of specific air pollutants in the development of congenital heart defects. (15)
Tips to reduce health risk in individuals exposed to air pollution
- Stay Indoors on High Pollution Days: Limit outdoor activities, especially physical exertion, on days with high pollution levels, particularly near pollution sources.
- Reduce Outdoor Air Infiltration: Minimize the entry of outdoor air pollutants into indoor spaces by closing windows and using weatherstripping to seal gaps.
- Use Air Purifiers: Install air filters or purifiers in indoor spaces to reduce the concentration of airborne pollutants like particulate matter (PM) and volatile organic compounds (VOCs).
- Consume Sulforaphane-Rich Foods: Include foods high in sulforaphane-based antioxidants, such as broccoli, cabbage, cauliflower, and Brussels sprouts, to help counteract the oxidative stress caused by pollution.
- Fish Oil Supplementation: Consider fish oil supplements, which are rich in omega-3 fatty acids, known for their anti-inflammatory properties that may help protect against pollution-related cardiovascular issues.
- Use Respirators or Face Masks: On days with high air pollution, especially if you are outdoors, use a respirator or face mask designed to filter out particulate matter (PM) and other harmful pollutants.

Conclusion
Experimental studies have shown a direct relationship between cardiovascular diseases (CVD) and air pollution, particularly smog. Fine particulate matter (PM) and carbon monoxide (CO) have been linked to several cardiovascular conditions, including acute myocardial infarction (AMI), arrhythmias, heart failure, cardiac arrest, and congenital heart defects. These pollutants contribute significantly to overall mortality. While large-scale societal interventions are most effective in combating the health effects of air pollution, individuals can take personal steps to reduce their risk of exposure and protect their cardiovascular health.
Refrences
1. (http://creativecommons. org/licenses/by-nc-nd/4.0/)
2.HTTPs://www.ahajournals.org/doi/full/10.1161/01.CIR.0000128587.30041.C8#core-R5-148593
4. https://www.sciencedirect.com/science/article/pii/S1538783622081181#bb0185
5.https://www.sciencedirect.com/science/article/pii/S1538783622081181#bb0190
6. https://www.sciencedirect.com/science/article/pii/S1538783622081181#bb0195
7.https://www.sciencedirect.com/science/article/pii/S1538783622081181#bb0200
8. https://www.sciencedirect.com/science/article/pii/S1538783622081181#bb0210
9. https://www.sciencedirect.com/science/article/pii/S1538783622081181#bb0215
10.https://www.sciencedirect.com/science/article/pii/S1538783622081181#bb0215
11.https://ehp.niehs.nih.gov/doi/abs/10.1289/ehp.7550
12. https://jech.bmj.com/content/62/3/267.short
14.https://www.atsjournals.org/doi/abs/10.1164/rccm.200412-1726OC
15.https://academic.oup.com/aje/article-abstract/155/1/17/134147
The article “Heart Under Siege” examines how air pollution harms cardiovascular health by causing oxidative stress, inflammation, and contributing to atherosclerosis. Pollutants like PM2.5 and nitrogen dioxide increase risks of heart attacks, strokes, and other heart diseases. It highlights vulnerable groups, such as the elderly and those with existing health issues, while stressing the importance of public health measures, lifestyle changes, and global efforts to reduce pollution.
So informative. Keep it up.
Your blog feels like a fountain of wisdom and inspiration. Thank you for offering it with us.
Your blog steadily engages my attention from start to finish. I find myself absorbed in every word you write.